The landscape of medical education has transformed to become more accessible. Traditional simulation training has long been constrained by physical infrastructure requirements, such as dedicated simulation centers, heavy equipment, and extensive staffing needs. However, the emergence of lightweight, portable simulation technology offers high-quality procedural training, particularly for residency programs in underserved regions and institutions with limited resources.
The Evolution of Accessible Simulation
For decades, medical simulation has been predominantly centralized in well-funded academic medical centers. These facilities house expensive mannequins, require dedicated space, and necessitate trained personnel to operate complex systems. While invaluable, this model creates inherent inequities. Residents at smaller programs, rural hospitals, or international institutions often lack consistent access to simulation-based training.
Portable simulation systems are changing this paradigm. Modern lightweight simulators can be transported in standard luggage or shipped to remote locations. This mobility fundamentally expands educational reach without compromising training quality.
Portable, High-Fidelity Training with the Miya Model
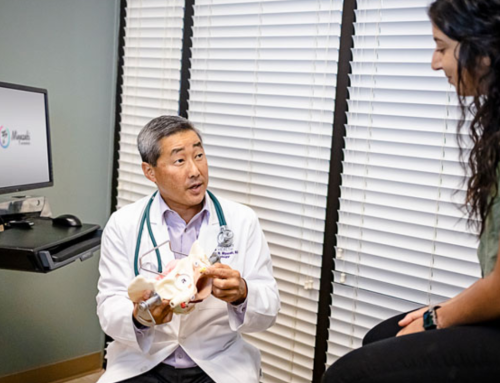
The Miya Model, developed by Miyazaki Enterprises, exemplifies how portable simulation can deliver realistic training without extensive infrastructure. Created by Dr. Douglas Miyazaki after observing vaginal surgery skills training needs among residents, this lightweight pelvic surgery simulator was developed specifically to address training gaps in obstetrics and gynecology residency programs.
Mounted on a rotating stand with convenient transportation, setup, use, and storage capabilities, the model provides realistic anatomical landmarks, tissue planes, and tactile feedback that closely mimics live surgical experience. The system’s portability has enabled training across numerous residency programs throughout the United States and in international hysterectomy training courses, bringing standardized, high-quality training to diverse educational settings.
Key Advantages of Portable Simulation Technology
Minimal Infrastructure Requirements
Some portable systems need adequate lighting, table space, and in some cases, standard electrical outlets. The Miya Model requires only surgical instruments and suture to perform multiple procedures at one setting, transforming conference rooms, empty offices, or hotel spaces into functional training environments within minutes.
This simplicity allows programs to convert existing spaces into temporary simulation laboratories without the expense of dedicated facilities. For vaginal hysterectomy training, residents can practice the following with the Miya Model:
- Clamping
- Cutting
- Tying pedicles
Reduced Proctor Dependencies
One of the most significant advantages of modern portable simulation is the decreased reliance on specialized personnel. Miyazaki Enterprises offers a comprehensive surgical curriculum, including setup instructions, best practices for training, and cleanup procedures, enabling programs to implement structured training with minimal faculty burden. The system’s design allows supervising physicians to guide multiple learners simultaneously while conducting objective assessments. The Miya Model App has videos and specific information for a variety of surgical procedures.
Contemporary portable simulators increasingly incorporate:
- Self-guided learning modules with embedded instruction
- Standardized curricula that reduce preparation time for faculty
- Objective assessment metrics through validated scoring systems
- Video recording capabilities for independent review and feedback
This autonomy allows residents to engage in deliberate practice during downtime, night shifts, or scheduled independent learning time without requiring a faculty member’s constant presence. When faculty oversight is beneficial, a single instructor can efficiently supervise multiple learners simultaneously, maximizing educational efficiency.
Scalability for Regional and Multi-Site Programs
Portable simulation enables consistent educational experiences across geographically dispersed locations.
Program directors using portable systems can:
- Rotate simulation equipment through affiliated hospitals on scheduled intervals
- Standardize procedural training across all sites using identical equipment
- Ensure rural or community hospital residents receive equivalent educational opportunities as their urban counterparts
- Conduct objective assessments using identical equipment and protocols
Enhanced Flexibility for Traveling Educational Courses
The portability revolution has particular implications for continuing medical education and specialty training courses. The American Board of Obstetricians and Gynecologists has approved vaginal hysterectomy and midurethral sling courses for Category I CME and Maintenance of Certification credits exclusively using the Miya Model since 2015. This distinction demonstrates how portable simulation can meet rigorous educational standards at professional conferences and traveling courses.
Conference organizers and medical educators can now offer hands-on procedural workshops at national meetings, international symposiums, or targeted regional training events without the prohibitive logistics of transporting full-scale simulation equipment. This mobility supports:
- Specialty society conference workshops with standardized, validated training models
- International training courses in resource-limited settings
- Regional skills courses for rural healthcare providers
- On-site training at community hospitals without established simulation programs
Clinical and Educational Outcomes
The benefits of portable simulation extend beyond convenience. Residents who have regular, convenient access to simulation equipment demonstrate improved procedural confidence, higher rates of skill retention over time, enhanced performance during initial supervised clinical procedures, and reduced complication rates in specific high-risk interventions.
Real-World Implementation: From Residency to CME
The American College of Obstetricians and Gynecologists has approved and accepted portable simulation models as methods for training gynecological exams and office procedures, with publicly available curricula covering basic examinations, including pap smears, endometrial biopsy, IUD placement, colposcopy, and cervical biopsy. This institutional endorsement demonstrates how portable simulation has transitioned from experimental technology to accepted educational standards.
These systems can be used for low-fidelity and high-fidelity training to meet a variety of training needs, with complete surgical curricula developed for main gynecological procedures. This flexibility allows programs to introduce simulation training early in residency using basic components, then progress to more complex, high-fidelity scenarios as learners advance.
The Future of Equitable Medical Education
The development and validation of systems like the Miya Model, supported by National Institutes of Health Small Business Innovation Research grants, demonstrates the scientific rigor underlying modern portable simulation technology. By removing geographical and institutional barriers, these tools ensure that a resident’s training quality isn’t determined by their program’s zip code or budget. As technology continues to advance and costs decrease, the vision of truly accessible, standardized procedural education for all residents becomes increasingly achievable. The question is no longer whether simulation improves training outcomes, but rather how we can ensure every resident, regardless of location or program size, has access to these proven educational tools.