THE MIYA MODEL
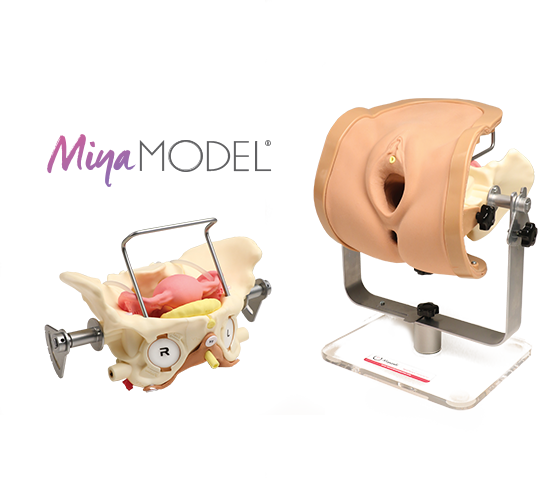
The Miya Model consists of a pelvic frame and multiple replaceable anatomic cartridges, designed with specific surgical procedures in mind. The model incorporates a number of features to simulate real surgical experiences, including lifelike skin and life-size organs, realistic cutting and puncturing tensions, palpable surgical landmarks, a pressurized vascular system that can simulate bleeding due to inadequate technique, and an inflatable bladder that leaks water if damaged.
Mounted on a rotating stand with the top of the pelvis open, the Miya Model is designed to provide access and visibility. This design enables supervising physicians and credentialing committees to have topical access and video capabilities, facilitating greater guidance and review. The lightweight model offers convenient transportation, setup, use, and storage. Currently, the Miya Model can be used to practice all major vaginal surgical procedures and has the potential to support additional procedures in the future.
The current standard for vaginal surgery instruction relies on both live surgery and the use of training cadavers. However, these approaches suffer from several handicaps, including patient risks, liability risks, availability limitations, high costs, and a high demand on proctoring surgeons. Over time, these limitations have led to a decrease in resident exposure to live training cases.In fact, Dr. Miyazaki conducted research at his home institution and found that the number of hysterectomies performed by residents has drastically decreased. Current residents are performing only about a quarter of the number of hysterectomies Dr. Miyazaki performed during his own residency just two decades ago. Trends in health care and a growing shortage in funding dollars suggest that this alarming dynamic will only continue to get worse.
These issues are not institution-specific and have become an ever-growing problem in residency programs across the country. Consequently, dramatic declines in surgical experience are generating a growing interest in the objective verification of minimal competency levels as residents graduate from one level to the next. This interest has prompted the Accreditation Council for Graduate Medical Education (ACGME) and the American Congress of Obstetricians and Gynecologists (ACOG) to develop and implement the Milestone Project. Despite the demands for increasing the quantity and quality of surgical training, as well as growing requirements for competency assessment and verification, neither the status quo of live surgeries and cadavers, nor other alternatives such as existing surgical simulators or anatomical models, are adequate solutions given the cost constrained environment.
The market demanded something different: a training tool that would provide lifelike quality, tactile feel, and meticulous anatomical placement, all while delivering cost efficiency, mobility, a low-risk environment, reproducibility, repetition of procedures and high-fidelity training–every time. After assessing these variables, Dr. Miyazaki determined that if designed appropriately, model-based simulation training could provide an ideal solution. He then put his innovative and entrepreneurial skills to work, and after more than six years of intense research, discovery, product development, testing, and validation, the Miya Model was born.
Supported Training & Procedures
The Miya Model is the only surgical simulation model that can support such a wide range of surgical training and procedures with the potential to add more in the future.
Basic Gynecological Examination
- Speculum exam
- Cervical visualization and pap smear
- Endometrial biopsy

Palpation of Key Surgical Landmarks
- Pubic tubercles
- Pubic rami
- Obturator fossa
- Arcus Tendineus Fascia Pelvis
- Ischial Spine
- Sacrospinous Ligament

Basic Gynecological Examination
- Total Vaginal Hysterectomy (with or without Bilateral Salpingo-Oophorectomy)
- Transoburator sling placement (both outside-in and inside-out approaches)
- Retropubic sling placement (both top-down and bottom-up approaches)
- Full thickness vaginal wall dissection to the Arcus Tendineus Fascia Pelvis
- Bilateral Sacrospinous Ligament Fixation Dilation and Curettage
- Uterine morcellation
- Dilation and Curettage
- Diagnostic Hysteroscopy
Miya Model Components
The Miya Model base model and cartridges were meticulously designed with high quality materials for realism, durability, and cost effectiveness.
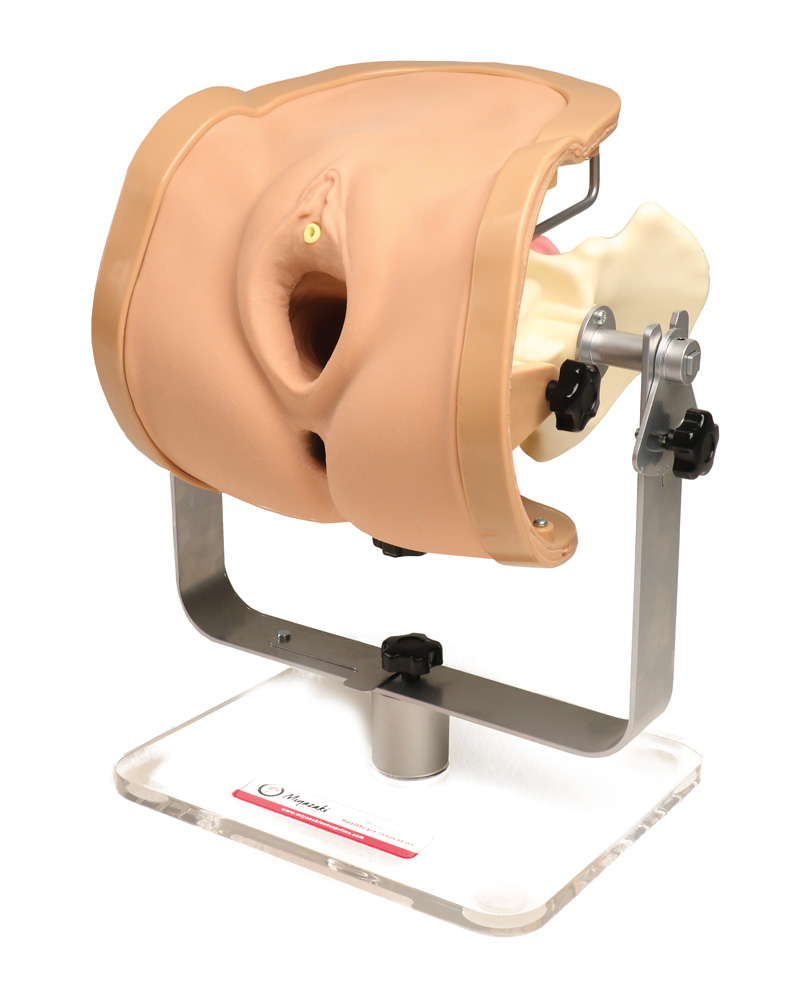
Vulva Assembly
- Realistic feel with self-healing properties
- Includes lower abdomen, vulva, urethral opening, vaginal introitus, anus and rectum
- Soft, life-like feel allows for palpation of bony landmarks such as: pubic tubercles, pubic rami, obturator fossa, ischial tuberosity and coccyx
- Medical grade silicone construction
- Realistic skin puncturing tension
- Urethral hole allows for catheterization
Pelvis
- Morphologically correct gynecoid pelvis
- Anatomically correct bony landmarks: pubic tubercles, pubic rami, obturator fossa, ischial spine, ischial tuberosity, and coccyx
- Patented replacement and locking systems for changing replaceable cartridges
- Open top design allows for easy part replacement and visualization
- Open side design to allow for lateral visualization
Stand
- 360-degree rotation
- Can be placed in Trendeienburg and reverse Trendeienburg position
- Pelvis can be locked into place for increased stabilization during simulations
- A C-clamp (not included) may be used to secure the simulator to a table or other surface

Vagina
- Realistic feel and vaginal texture
- Soft vaginal wall allows for palpation of Arcus Tendineus Fascia Pelvis (ATFP) from the inferior pubic ramus to the ischial spine
- Special materials design enables the surgeon to have a realistic feel when cutting with scissors or scalpel and suturing the vaginal wall
- Opens from the vulva at the pubic rami; the vagina widens and extends from arcus to arcus bilaterally, almost reaching the spines but stopping about 1 cm before the spinous process
- Anterior and Posterior cul-de-sacs are palpable
- Endopelvic fascial layer extends to the ATFP and is anchored to a slot above the ischial spines of the pelvis; this configuration creates a fascial plane and enables full-thickness vaginal wall dissection to the Arcus Tendineus Fascia Pelvis

Multi-Procedural Uterus
- Large high-fidelity uterus featuring a hollow gynecoid cavity and vasculature supply
- Mesh embedded in aspects of the uterosacral, cardinal, and broad ligaments to reinforce proper suture placement
- Anterior peritoneal flap signifies when an anterior cul-de-sac entry is performed
- Vascular supply supports bleeding with improper knot tying technique
- Realistic clamping, cutting, and suturing tensions
- Medical grade silicone construction
- Hollow gynecoid cavity allows for IUD insertion, uterine sounding and manipulation, endometrial biopsy, diagnostic hysteroscopy, and operative hysteroscopy with resection and electrocautery

Assessment Uterus
- High-Fidelity uterus with vascular supply
- Supports vaginal hysterectomy, apical suspension, bladder flap
dissection and anterior cul de sac entry - Medical grade silicone construction
- Realistic clamping, cutting, and suturing tensions
- Vasculature runs through the broad ligament and will fit standard IV
tubing - Mesh is embedded in aspects of the uterosacral, cardinal, and
broad ligaments to reinforce proper suture placement - Vascular supply supports bleeding with improper knot tying
technique - Anterior peritoneal flap signifies when an anterior cul de sac entry is
performed

Assessment Hysterectomy Set
- Bonded vagina and Assessment Uterus validated for objective assessment of vaginal hysterectomy
- Supports vaginal hysterectomy, anterior repair, posterior repair, full thickness vaginal wall dissection, retropubic slings, transobturator slings, and single incision slings
- Bonded high-fidelity (double layer) vagina and Assessment uterus
- Medical grade silicone construction
- NIH-supported validation studies demonstrated that the Assessment Hysterectomy Set can be used to objectively assess surgical competency of vaginal hysterectomy (this study was published in the ACOG Green Journal and is available with open access)

Bladder
- Hollow bladder with opening on top for filling with water, grommet, and plug
- Expands to hold 100 cc of fluid, leaks when punctured
- Deflates when empty
- One way valve in urethra simulates sphincter and allows for cauterization, accepts 12-16fr catheter
- Attaches anteriorly to groove in pubic bone and fits snugly between pubic bone and uterus

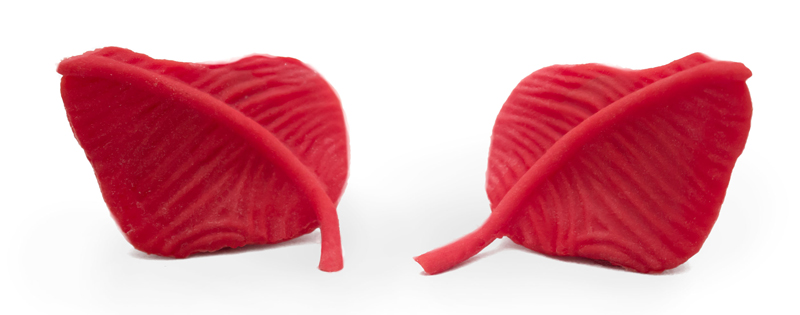
Sacrospinous Ligament
- Single band with hook connections at each ischial spine and screw on sacral plate
- Simulates ‘pop’ of puncture with trocar passage
- SS ligament has the ‘characteristic’ ridges which are palpable on the vaginal and rectal exam
- The ligament originates from the ischial spine and terminates into the lateral sacrum
- Trocar/needle passage can be from above or below the ligament
- Sacral edge lines up with foramina S4-S5, about 3 cm wide as per cadaver studies; prominent texture can be felt through the vaginal wall
Obturator Complex
- Combined obturator membrane and obturator internus/externus muscles
- Obturator fossa is easily palpated
- 360 degrees of tension during palpation
- Obturator complex is housed with a circular frame which turns and locks into the pelvic sidewall at the obturator foramen
- Special locking mechanism allows for realistic trocar passage feel and ‘pop’ from an inside out or outside in approach
- Includes raised ridge of the ATFP which extends from the inferior pubic rami towards the ischial spine
- Anchoring devices and suturing can be performed along the length of the ATFP
- Simulates “pop” of puncture




